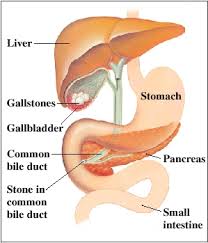
Pancreatitis is an inflammation of the pancreas. The pancreas is an organ that lies near the stomach. It is responsible for secreting digestive enzymes into the small intestine. It is also responsible for glucose homeostasis by secreting insulin and glucagon in response to changes in blood glucose levels. Pancreatitis can develop can develop acutely, last for days, and then resolve. Repeated episodes of acute pancreatitis can lead to the development of chronic pancreatitis. The symptoms of chronic pancreatitis include upper abdominal pain that may radiate to the back, nausea, vomiting and weight loss. As the function of the pancreas begins to decline, digestion is altered and stool becomes oily and smelly. Diabetes Mellitus may develop as insulin and glucagon production are affected. Chronic pancreatitis is most commonly caused by alcohol ingestion, cystic fibrosis and pancreatic cancer. Gallstones, elevated levels of calcium and triglycerides in the blood are also associated with pancreatitis. The diagnosis of chronic panceatitis is made by history and physical exam. Blood work is useful to look for elevated levels of lipase and amylase which are pancreatic enzymes. CT scan, MRI scan and ultrasound examinations are useful to look for damage of the pancreas and to exclude other causes of abdominal pain. Treatment of chronic pancreatitis includes pain medications and supplementation of pancreatic enzymes. A celiac plexus block by an interventional pain management physician is used to block pain impulses from the pancreas and decrease pain.